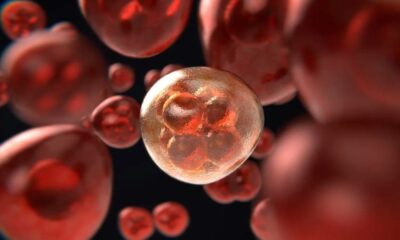
Hematology
Millions could be Saved by Reevaluating the Delivery of Cancer Immunotherapy Medications
-

 Diabetology2 weeks ago
Diabetology2 weeks agoDiabetes Screening: Why Early Detection Saves Lives
-

 Diabetology2 weeks ago
Diabetology2 weeks agoCaring for Diabetes Daily: A Practical Guide to Routine Control
-

 Diabetology1 week ago
Diabetology1 week agoGlycemic Index Chart + Tips: Best & Worst Foods for Blood Sugar
-

 Diabetology2 weeks ago
Diabetology2 weeks agoHyperglycemia: What You Need to Know to Stay Safe
-

 Diabetology1 week ago
Diabetology1 week agoDaily Diabetes Management Plan for Type 2 Diabetes
-

 Diabetology1 week ago
Diabetology1 week agoUnderstanding the Impact of High Glucose Levels
-

 Diabetology5 days ago
Diabetology5 days agoHow Real-Time Blood Glucose Monitors Improve Health Outcomes
-

 Diabetology5 days ago
Diabetology5 days agoHow a Plant-Based Diet Can Help Manage Type 2 Diabetes