Cancer cells that are rapidly multiplying make up tumors. Therapeutic targets can be identified by gaining an understanding of the biochemical processes that drive their unstoppable growth.
Specialists from Washington University in St. Louis have developed a technology to study tumor growth in another dimension; literally. The researchers established a new technique to watch what nutrients are used at which rates spatially all through a tissue.
They identified pathways whose activity is elevated in a particular way in brain cancer by employing this multidimensional imaging approach, which provided clues for potential treatment options. Nature Communications carried the study’s May 19 publication date.
The new study’s senior author is Patti, who also works as a researcher at the Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine.
Human biology is fundamentally 3D in nature. The arising field of spatial biology means capturing this geometry by imaging the locations of genes, proteins, and metabolites. Patti and colleagues’ method covers fluxes, the rates at which molecules in cells undergo a transformation, in addition to spatial profiling.
“Other technologies provide what is essentially a roadmap of biochemistry. Our goal was to add in a measurement of how fast traffic is flowing on the different roads,” Patti said.
By Patti’s analogy, the new strategy is much the same as the feature in Google Maps that uses green and red colors to show the density of cars on a given road.
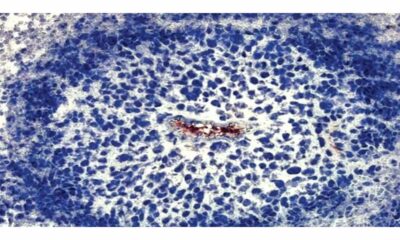
The researchers created a high-resolution map of the “tumor ecosystem” using a human glioblastoma mouse model. Because of this, they were able to identify which molecules were situated in which regions of the brain and how rapidly those molecules were transforming into other things.
The findings shed light on how brain tumor cancer cells acquire lipids, a fundamental fat component.
A cell’s membrane—its outermost covering—cannot be constructed without lipids. As cancer cells multiply, they need lipids to encase the new cells. Patti’s earlier research had demonstrated that cancer cells prefer to scavenge lipids from their local environments. Yet, that was when cancer cells were cultured in isolation with lipids present in the media.
The new study demonstrated that brain cancer cells typically generate the lipids they require for growth rather than stealing them.
“The brain is a unique environment. The availability of lipids is more limited than in other tissues where tumors reside,” Patti explained.
The speed at which a few lipids were synthesized was basically as much as 8-fold higher in brain tumors contrasted and surrounding healthy tissue. Although the exact magnitude of the increase varied, the pattern in cancer cells throughout the tumor was surprisingly consistent.
“A single tumor can span multiple different environments. The center might be hypoxic, while the outside is in contact with healthy tissue,” Patti said. “You might have predicted differences between these different regions, but we didn’t observe any patterns like that.”
This finding is significant on the grounds that realizing that cancer cells within brain tumors depend on a similar biochemical pathway to fuel their development implies that researchers could target it to slow or stop sickness movement.
“When a pathway is more active, its flux goes up. That makes it a good candidate for therapeutic intervention,” Patti said. “We are excited about testing whether impairment of fatty acid elongation will be effective in treating mouse models of disease.”

 Diabetology2 weeks ago
Diabetology2 weeks ago
 Diabetology2 weeks ago
Diabetology2 weeks ago
 Diabetology2 weeks ago
Diabetology2 weeks ago
 Diabetology1 week ago
Diabetology1 week ago
 Diabetology2 days ago
Diabetology2 days ago
 Diabetology2 days ago
Diabetology2 days ago
 Diabetology2 days ago
Diabetology2 days ago
 Diabetology9 hours ago
Diabetology9 hours ago