A large UK Biobank study, which was recently published online in the journal Heart, suggests that despite traditional underlying risk factors, cancer survivors may have a higher long-term risk of subsequent cardiovascular disease.
The findings suggest that people who have had breast or blood cancer in the past may be at greatest risk.
Shared vascular risk factors as well as the treatments and biological processes related to the cancer itself are completely connected with an increased risk of incident cardiovascular disease among cancer survivors, note the scientists.
However, the majority of the evidence to date suggests that the first year following diagnosis is when cardiovascular complications are most likely to occur. Few studies have included cardiovascular imaging to pinpoint damage to the cardiovascular system that has not yet manifested as symptoms or considered potential risks over the longer term.
The researchers compared the cardiovascular health of 18,714 UK Biobank participants with a prior diagnosis of a common cancer—lung (313), breast (9531), prostate (3291), blood (2230), womb (937), or bowel (2412)—with the cardiovascular health of the same number of UK Biobank participants without a prior cancer diagnosis and matched for age and traditional vascular risk factors in order to fill in these knowledge gaps.
The majority of the participants were female, with an average age of 62. Using linked health records, their cardiovascular health was monitored for nearly a decade.
Factors related with more terrible cardiovascular health, including smoking, high blood pressure, and excess weight were common among those with a past cancer diagnosis. Diabetes was present in nearly one in ten people who had lung, womb, or bowel cancer. Prior cardiovascular disease was additionally somewhat common (18%; 3289).
During the monitoring period, almost a third of cancer survivors experienced one of the following: ischaemia of the heart; stroke; unusual heart rhythm (atrial fibrillation); cardiovascular breakdown; mechanical or electrical signaling problems with the heart (non-ischaemic cardiomyopathies); blood clots in the veins, arteries, or lungs; pericarditis is an inflammation of the heart’s lining.
Lung, blood, and prostate cancer patients had the highest rates of new cardiovascular disease (49.5%), with ischaemic heart disease, atrial fibrillation, and heart failure being the most common cardiovascular diseases among all cancers.
19% of cancer survivors died during the monitoring period, compared to 8.5% of the comparison group. One in every 12 people who survived cancer died from cardiovascular disease.
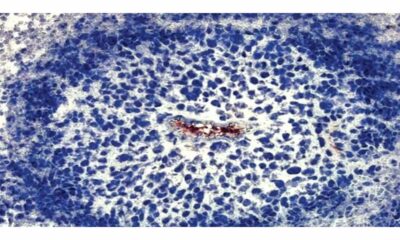
MRI scan results for 1354 study participants also revealed that, regardless of underlying vascular risk factors, the size and function of the heart had significantly deteriorated in cancer survivors.
Blood cancer survivors had altogether expanded risks of developing all the cardiovascular disease types considered contrasted and their peers without cancer. MRI scans also revealed clinically significant changes in their hearts’ size and function.
According to the researchers, patients with blood cancer are exposed to chemotherapies that are known to be harmful to heart tissue as well as radiotherapy that targets the chest wall over the heart.
In a similar vein, people who had breast cancer were more likely to be diagnosed with pericarditis, have heart failure, or die from non-ischaemic cardiomyopathies. Their scans were additionally bound to show proof of functional heart changes.
“These observations likely reflect cardiotoxicity linked to breast cancer therapies,” point out the researchers, adding that these people were also 8 times more likely to die of disease associated with high blood pressure.
This is an observational study, and accordingly, can’t establish cause. In addition, the researchers acknowledge a number of limitations to their findings, such as the lack of information on cancer grade, stage, or specific treatment options and the small number of lung and womb cancer survivors.
They note that because the majority of participants in the UK Biobank study are White, the findings may not apply to people of other ethnic backgrounds.
Nonetheless, they conclude: “Importantly, we demonstrate that past cancer confers an increased risk of cardiovascular events, independent of traditional vascular risk factors and that this risk may extend several years beyond the initial cancer diagnosis.”
Their findings show “particular vulnerability of individuals with past breast and haematological cancer, who appeared at greatest risk, both with regards to the risk of incident clinical disease and adverse cardiac remodeling,” they add.
Professor José Banchs from the University of Colorado School of Medicine in the United States and Dr. Tara Lech from Beth Israel Lahey Health emphasize in a related editorial: “The importance of heart disease in patients undergoing cancer care cannot be understated, but also how critical it becomes to prioritise a care continuum after cancer is survived.
“The fantastic progress in the treatment and even cure of malignancies has undoubtedly highlighted the need for post cancer care like never before,” paving the way for more tailored care, they write.

 Diabetology1 week ago
Diabetology1 week ago
 Diabetology5 days ago
Diabetology5 days ago
 Diabetology1 week ago
Diabetology1 week ago
 Diabetology7 days ago
Diabetology7 days ago
 Diabetology1 week ago
Diabetology1 week ago
 Diabetology5 days ago
Diabetology5 days ago
 Diabetology3 days ago
Diabetology3 days ago
 Diabetology3 days ago
Diabetology3 days ago